Course description
The Study of Anatomy, Vaccination and Penicillin:
Game Changers for our Life Expectancy
 In this lecture, we will look at three areas of science that forever changed the way we practice modern medicine. There is, sadly, no time to look at Hippocrates or Ibn Sina or a hundred other great contributors to our understanding of the ways our bodies work… but this may give you a taste of the history of medicine. The topics are: the history of anatomy; vaccination and immunization; and the discovery of penicillin.
In this lecture, we will look at three areas of science that forever changed the way we practice modern medicine. There is, sadly, no time to look at Hippocrates or Ibn Sina or a hundred other great contributors to our understanding of the ways our bodies work… but this may give you a taste of the history of medicine. The topics are: the history of anatomy; vaccination and immunization; and the discovery of penicillin.
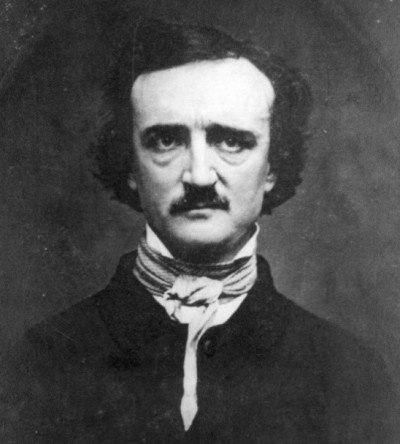
Galen, who lived from 129 AD to between 200 and 216, is known as the father of anatomy (or the study of the human body). His classic textbook was re-discovered in Western Europe in the fourteenth century and was still used in the sixteenth. It was so highly regarded that at least two people were publicly burnt for criticizing some of Galen’s findings.
Galen was born in (what is now) Turkey, a part of the Roman Empire and, for four years, was doctor to the gladiators at the time of the Emperor Marcus Aurelius. (This was exactly the same period as the action of the Hollywood film called ‘Gladiator’, starring Russell Crowe.) During his four years in this job, only four gladiators died under his knife. He went on to become Emperor Commodius’ doctor and also understood the importance of diet, physical exercise and hygiene for health.
It is, therefore, surprising that Galen never dissected a human body. This was forbidden at the time. He only practiced his skills on pigs and monkeys, but as everyone thought that their bodies were the same as human ones, nobody saw this as a disadvantage.
 Of course, there were many mistakes in Galen’s book but professors of medicine in Europe in the Middle Ages did not mention these for years when they looked at human corpses. Students knew that if they wanted to pass their university exams and become doctors, they had to copy what Galen had written in his book and pay no attention to what they could see with their own eyes in their anatomy lessons.
Of course, there were many mistakes in Galen’s book but professors of medicine in Europe in the Middle Ages did not mention these for years when they looked at human corpses. Students knew that if they wanted to pass their university exams and become doctors, they had to copy what Galen had written in his book and pay no attention to what they could see with their own eyes in their anatomy lessons.
Andreas Vesalius (1514 – 1564) changed all that. He found more than two hundred mistakes in Galen’s work and, perhaps because he was Emperor Charles V’s doctor, had the courage to publish them. This made him very unpopular. A British surgeon, William Harvey (who lived from 1578 till 1657), corrected Galen’s studies of the heart. However, both Vesalius and Harvey had a similar problem to Galen: although they could dissect human bodies, very few people offered their corpses to medical science. (Harvey actually dissected both his own father and sister to learn more.)
 Perhaps, the artist William Hogarth’s picture of a dissection room explains why: they were dirty – Hogarth’s picture even shows a dog in the room looking hungrily at a human heart – and showed no respect to the dead person. Only hanged murderers’ bodies could be cut up and hospitals got four bodies a year. Because of this, doctors advertised public dissections in halls and paid for dead bodies. They could not be choosy because there were never enough and so they did not always ask where the bodies came from.
Perhaps, the artist William Hogarth’s picture of a dissection room explains why: they were dirty – Hogarth’s picture even shows a dog in the room looking hungrily at a human heart – and showed no respect to the dead person. Only hanged murderers’ bodies could be cut up and hospitals got four bodies a year. Because of this, doctors advertised public dissections in halls and paid for dead bodies. They could not be choosy because there were never enough and so they did not always ask where the bodies came from.
Of course, this situation meant bodies were stolen from their graves as soon as they were buried and some people were actually murdered so that their bodies could be sold to doctors.
In 1828, two Irish hotel keepers, William Burke and William Hare, sold the body of a guest who had died in the night to a doctor and earned so much money from it that they then went on to murder sixteen people.
Nobody asked any questions until a dead body was found under a bed in their hotel. Burke was hanged, his body was dissected and his skin used as leather. Because Hare co-operated with the police, they set him free. But the murders were useful in one way because the government finally realized the importance of dissection to medical science and changed the law so that they could use the bodies of poor people who had no families.
Nowadays, the geography of the human body is well-understood and anatomy offers few new insights. However, it is still useful for eighteen-year-old medical students straight from secondary school who, for the first time in their lives, come face to face with terrible injuries and diseases. The dissecting room is where they get used to blood and the surgeon’s knife.
The next innovation was the importance of vaccination in preventing disease through immunization.
 In about 1920, medicine cured more people than it killed for the first time in history. Hospitals were very dirty and it was possible for patients to get serious infections and die. The same was true in operating theatres, although they were starting to get cleaner. The most important reasons that medicine got better were antibiotics and, vitally, immunization.
In about 1920, medicine cured more people than it killed for the first time in history. Hospitals were very dirty and it was possible for patients to get serious infections and die. The same was true in operating theatres, although they were starting to get cleaner. The most important reasons that medicine got better were antibiotics and, vitally, immunization.
Immunizations came very late to Europe. It was the late eighteenth century before a country surgeon called Edward Jenner tried immunizing an eight-year-old boy called James Phipps against smallpox. This disease killed many, many people every year and also blinded thousands of others. Jenner noticed that women working on dairy farms never caught the disease. Because he was a country doctor, he probably also heard about farmers making cuts on healthy people and putting scabs from sick people into these wounds. This was not enough to make healthy people sick but it stopped them getting seriously ill later with smallpox. Nobody knew why this worked but people who travelled around Britain used it.
In fact, the British Army in India knew that the Moghuls made cuts on their soldiers’ arms and put scabs from people who had smallpox on these. The wife of the British Ambassador to the Ottoman Empire, Lady Mary Montagu, had seen this in Istanbul decades before and did the same to her own children, but it never became popular at home.
 The reason Jenner’s answer was different was that he discovered cows had a different disease from smallpox, called cow pox, which many women on farms caught. However, it was not serious in human beings and so the girls could continue to work and, later, never got the often fatal disease, smallpox. He also found that the disease could travel from cows to people and from one person to another. He then made a vaccine. (Interestingly, the word ‘vaccination’ comes from the Latin word ‘vacca’, meaning ‘cow’.)
The reason Jenner’s answer was different was that he discovered cows had a different disease from smallpox, called cow pox, which many women on farms caught. However, it was not serious in human beings and so the girls could continue to work and, later, never got the often fatal disease, smallpox. He also found that the disease could travel from cows to people and from one person to another. He then made a vaccine. (Interestingly, the word ‘vaccination’ comes from the Latin word ‘vacca’, meaning ‘cow’.)
In 1840, the British Parliament offered free vaccinations to the poor, but very few people used these. Thirteen years later, they had to use them. However, the poor were not happy about the new law and they fought against it and many people were killed. They could not understand why only poor people needed vaccinations. Also, they did not want travelling doctors to make cuts on their month-old babies’ arms and then put smallpox scabs into them. The babies often became sick. The officials used knives that were not clean and open cuts often killed their children because people could not keep the wounds clean. The same thing happened in Indian villages. People welcomed vaccination when smallpox was killing thousands, but did not want it when everyone was healthy.
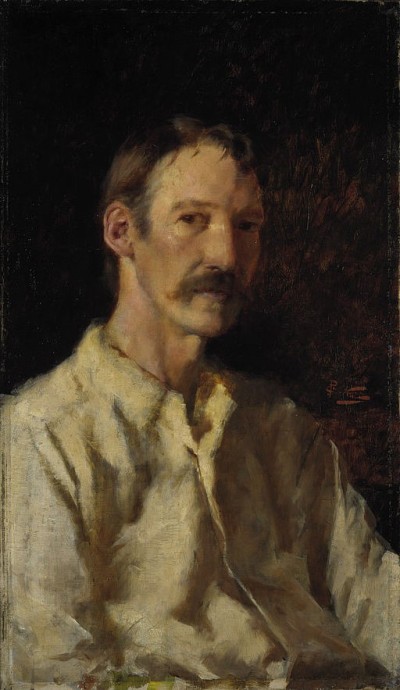
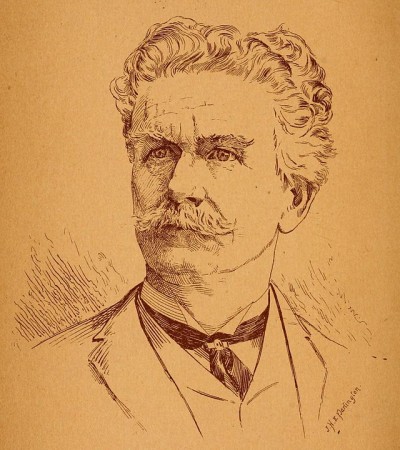
 In France, Louis Pasteur (1822 – 1895) was also working on making vaccines for rabies. His method was different. He made rabbits sick with the disease and then did the same with the next generation of rabbits, and the next and the next. Of course, later generations could fight the disease better and so did not die. Pasteur then took blood with a weak form of the disease from these rabbits and used it to vaccinate people against rabies.
In France, Louis Pasteur (1822 – 1895) was also working on making vaccines for rabies. His method was different. He made rabbits sick with the disease and then did the same with the next generation of rabbits, and the next and the next. Of course, later generations could fight the disease better and so did not die. Pasteur then took blood with a weak form of the disease from these rabbits and used it to vaccinate people against rabies.
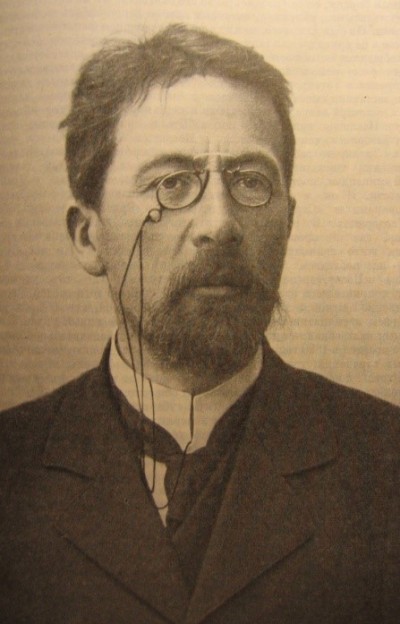
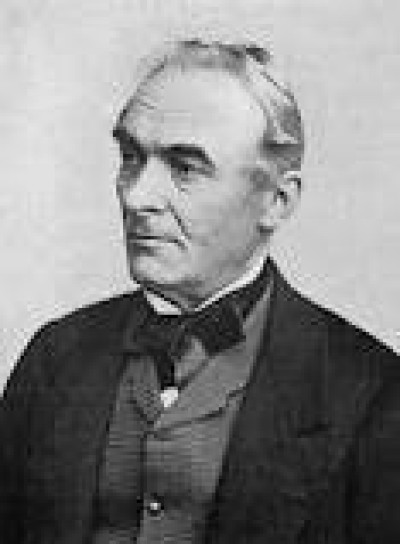
A man that Pasteur hated, the German scientist Robert Koch (1843 – 1910), was also working on a vaccination against an often fatal disease, tuberculosis (also called TB). In 1884, he wrote four ‘postulates’, which are now the basis of the science of immunology:
1.The TB micro-organism must be found in large numbers in all bodies with the disease but never in healthy bodies
2.The micro-organism must be isolated from other cells and grown in a pure culture
3.The micro-organism grown in the culture should lead to TB when it is put into a healthy body
4.The micro-organism found in the newly-diseased body must again be isolated and shown to be exactly the same as the original TB micro-organism.
(Although Koch was talking especially about TB and cholera, the postulates are true of any disease.)
You will see that the first, second and last of Koch’s postulates use the word ‘must’ but the third one has ‘should’ instead. This is because Koch showed that not all healthy bodies will get cholera or TB when micro-organisms are put in them.
 It was not until 1891 when Ilya Mechnikov explained the importance of the immune system in fighting diseases that Koch's work was recognised and he won the Nobel Prize for Medicine in 1905. Mechnikov then won it in 1908.
It was not until 1891 when Ilya Mechnikov explained the importance of the immune system in fighting diseases that Koch's work was recognised and he won the Nobel Prize for Medicine in 1905. Mechnikov then won it in 1908.
It is interesting to see that, although immunisation has been vital in controlling disease, it has only cured smallpox. The last case in the world was in Somalia in 1977.
Finally, we can move to the twentieth century and survey Fleming’s discovery of penicillin, a game-changing drug that has forever altered the treatment of infections.
At the beginning of the twentieth century, American men could expect to live to forty-six and women to forty-eight years of age. The main cause of death was infectious diseases, not cancer and heart attacks as it is today. Operations were very, very dangerous because so many people died of infections after they left the operating room.
After the Second World War, when doctors started to use penicillin with their patients, all that changed. Very soon, men and women could expect more than seventy years of life. Some infectious diseases continued to kill but much, much less often than before. And we did not need to worry about dying after an operation. The main cause of death became non-communicable disease, like heart attacks and cancer. All because of penicillin.
However, it was only because of a series of accidents that doctors could give penicillin to their patients. Even the discovery of penicillin was just luck!
This is how it happened.
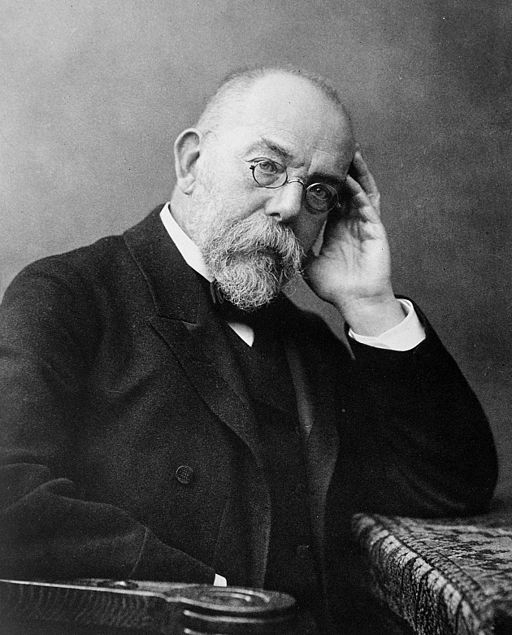
 Alexander Fleming, a Scottish doctor, was interested in developing a medicine that could fight bacteria. As a doctor in the First World War, he saw hundreds of young soldiers die because they got bacterial infections. He knew that bacteria were killing countless thousands and he tried through his research to find an answer.
Alexander Fleming, a Scottish doctor, was interested in developing a medicine that could fight bacteria. As a doctor in the First World War, he saw hundreds of young soldiers die because they got bacterial infections. He knew that bacteria were killing countless thousands and he tried through his research to find an answer.
But everyone needs a break and, in August 1928, Dr. Fleming took a well-earned holiday with his four-year old son, Robert, and wife, Sarah. Alexander Fleming was a very hard-working and sometimes brilliant researcher, but he had a fault – he was really untidy, not just at home but in his laboratory as well. When Fleming arrived back at his laboratory on 3rd September, he saw that a petri dish was covered in fungus. He forgot to wash it before he went on holiday a month before. But there was another thing he noticed: the staphylococci bacteria around the fungus were dead. In the other petri dishes, the staphylococci were the same or bigger than they were before he left for his holiday. “That’s funny!”, Fleming famously said.
By the end of the month, Fleming knew that the mould came from the scientific family Penicillium and he realized it could kill many, many different types of bacteria.
There were difficulties though. First, when Fleming wrote his article on penicillin, nobody paid attention. He was a very poor talker and writer and he could not show people the truth and importance of his discovery. Next, it was very hard to grow penicillin mould and even harder to isolate it.
 For all these reasons, Fleming decided that penicillin was not going to make a major difference to human health. He turned his attention to other things.
For all these reasons, Fleming decided that penicillin was not going to make a major difference to human health. He turned his attention to other things.
Luckily, two other scientists, Howard Florey and Ernst Boris Chain, who were working at Oxford University, did not give up on the problem of how to mass-produce penicillin. The start of the Second World War and the probable deaths of so many soldiers from bacterial infections also meant that both the British and US governments made sure that the scientists had the cash to speed up their research. Florey’s and Chain’s first successful results were published in 1940. Fleming immediately telephoned them to arrange a meeting. This surprised the scientists because they thought Fleming was dead.
Mass production of penicillin began in 1942.
 At first, penicillin was used only for wounded soldiers or those suffering from sex diseases. However, in 1945, it became available for the general public and changed public health forever.
At first, penicillin was used only for wounded soldiers or those suffering from sex diseases. However, in 1945, it became available for the general public and changed public health forever.
Nowadays, we are again worried about infections because there are super-bacteria that penicillin cannot kill. Fleming realized – even in 1945 – that this could happen. He said again and again that doctors must not give penicillin for every minor medical problem – only for bacterial infections. He also made it clear that patients needed to take penicillin for long enough and in big enough quantities to kill bacteria or they would come back stronger than before! But people did not listen! Now, we need to develop new drugs again.
Fleming died in 1955 of a heart attack. He won the Nobel Prize in 1945 (with Florey and Chain) after becoming Sir Alexander the year before. He was a legend in the scientific world but he never took this seriously. He always said Florey and Chain were the heroes and that his own reputation was ‘the Fleming myth’.
If you want to watch some videos on this topic, you can click on the links to YouTube videos below.
If you want to answer questions on this article to test how much you understand, you can click on the green box: Finished Reading?
Videos :
1. The story of Alexander Fleming and Penicillin for Children (7:43)
2. The Origin of Vaccines (2:30)
3. How Penicillin Changed the World (2:09)
4. Ancient Rome’s most Notorious Doctor (5:10)

 In this lecture, we will look at three areas of science that forever changed the way we practice modern medicine. There is, sadly, no time to look at Hippocrates or Ibn Sina or a hundred other great contributors to our understanding of the ways our bodies work… but this may give you a taste of the history of medicine. The topics are: the history of anatomy; vaccination and
In this lecture, we will look at three areas of science that forever changed the way we practice modern medicine. There is, sadly, no time to look at Hippocrates or Ibn Sina or a hundred other great contributors to our understanding of the ways our bodies work… but this may give you a taste of the history of medicine. The topics are: the history of anatomy; vaccination and  Of course, there were many mistakes in Galen’s book but professors of medicine in Europe in the Middle Ages did not mention these for years when they looked at human
Of course, there were many mistakes in Galen’s book but professors of medicine in Europe in the Middle Ages did not mention these for years when they looked at human Perhaps, the artist William Hogarth’s picture of a
Perhaps, the artist William Hogarth’s picture of a  In about 1920, medicine cured more people than it killed for the first time in history. Hospitals were very dirty and it was possible for patients to get serious
In about 1920, medicine cured more people than it killed for the first time in history. Hospitals were very dirty and it was possible for patients to get serious  The reason Jenner’s answer was different was that he discovered cows had a different disease from
The reason Jenner’s answer was different was that he discovered cows had a different disease from  In France, Louis Pasteur (1822 – 1895) was also working on making vaccines for
In France, Louis Pasteur (1822 – 1895) was also working on making vaccines for 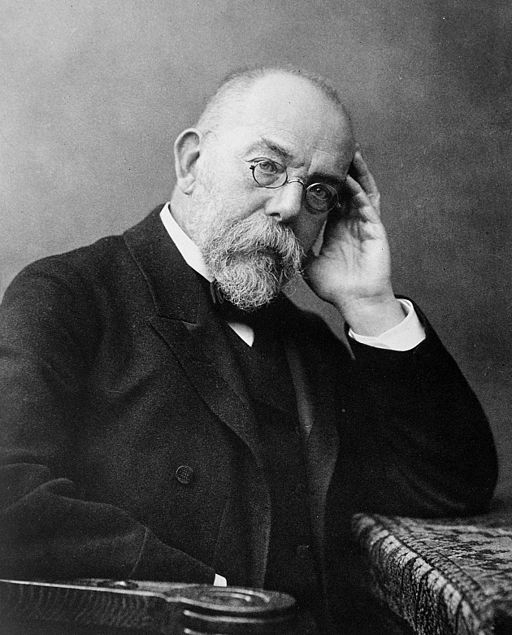 It was not until 1891 when Ilya Mechnikov explained the importance of the immune system in fighting diseases that Koch's work was recognised and he won the Nobel Prize for Medicine in 1905. Mechnikov then won it in 1908.
It was not until 1891 when Ilya Mechnikov explained the importance of the immune system in fighting diseases that Koch's work was recognised and he won the Nobel Prize for Medicine in 1905. Mechnikov then won it in 1908. Alexander Fleming, a Scottish doctor, was interested in developing a medicine that could fight
Alexander Fleming, a Scottish doctor, was interested in developing a medicine that could fight  For all these reasons, Fleming decided that penicillin was not going to make a major difference to human health. He turned his attention to other things.
For all these reasons, Fleming decided that penicillin was not going to make a major difference to human health. He turned his attention to other things. At first, penicillin was used only for
At first, penicillin was used only for